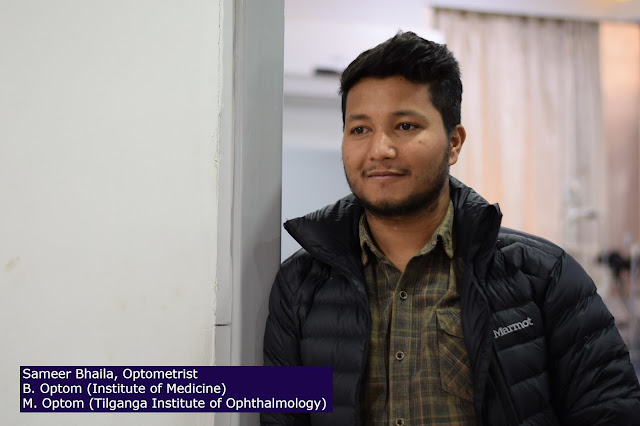
This article is written by Mr Sameer Bhaila, who is the graduate of master of optometry first batch from Tilganga Institute of Ophthalmology, a joint constituent campus of Pokhara University (PU).
Background:
Refractive surgery
‘Refractive surgery’ encompasses any
procedure that corrects refractive error, one of the leading causes of
reversible visual impairment in the world [1]. It is
now recognized that refractive surgery has significant impact on quality of life
and daily work, with benefits extending beyond spectacle independence [2]. Laser refractive surgery is recognized as an extremely
effective and safe procedure for low to moderate levels of refractive error [3], with more than 99.5% achieving spectacle independence [4]. The US FDA run Patient-Reported Outcomes with laser in situ
keratomileusis showed that, on average, 95% of patients were satisfied with
their treatment [5]. Today, refractive surgery has evolved
beyond the stereotypical ‘laser eye surgery’. Developments in femtosecond laser
technology have led to the improvement of laser in situ keratomileusis (LASIK)
and the birth of refractive lenticule extraction [6]. Novel refractive surgical implants have also been introduced,
ranging from intracorneal to intraocular implants. However, with laser
refractive surgery already achieving excellent clinical outcomes, it is often
difficult to demonstrate that these newer procedures are superior to the
established techniques [7]. Thus, the next frontier of refractive
surgery challenges clinicians and scientists to achieve outcomes superior to
the ‘traditional 20/20’, often used to depict ‘perfect’ uncorrected distance
visual acuity (UDVA). Technologies have been developed to enhance preoperative assessments
and imaging for better patient selection, there are now improved customized
treatments to specifically correct ocular aberrations, and novel techniques to
adapt to dynamic refractive changes in the
eye such as presbyopia. In this review, we summarize the evolution of
refractive surgery, which now ranges from keratorefractive procedures to
refractive lens exchange. Each section will discuss historical development,
recent advancements, and possible progress into the future beyond 2020.
Preoperative
evaluation for refractive surgery
Traditionally, refractive surgery may be
considered as two major sub-disciplines, which can be applied jointly in some
cases to correct complex refractive errors: keratorefractive or intraocular
lens (IOL)-based surgery. Keratorefractive surgery involves altering the
corneal surface shape; while with IOL-based surgery, an IOL implant is added to
the optical elements. Corneal topography provides an assessment of corneal
surface shape, while wavefront analysis provides an assessment of image
formation by the entire eye’s optical system. Conventionally, these
investigations have been routinely used in preoperative evaluation for
refractive surgery. Placido-based curvature topographic systems are valuable
tools in gauging the corneal curvature and refractive status, but do not
directly portray the actual shape of the cornea [8].
Scheimpflug corneal tomography is a 3-D imaging technique that characterizes
the anterior/posterior corneal surfaces, along with corneal thickness
distribution. Preoperative assessment is important to exclude any
contraindicated corneal conditions, while detection of subclinical keratoconus
suspects is crucial to prevent iatrogenic postsurgical ectasia [9]. Integrating data derived from corneal topography, biometry, and
wavefront analysis can also help clinicians validate decisions about customized
refractive surgery treatments and IOL power selection.
Beyond
corneal topography: Biomechanics and high-resolution imaging
Recently, the addition of corneal
biomechanics to corneal topography has been studied as a potential adjunct to
preoperative evaluation for keratorefractive procedures. The corneal
visualization tonometer (Corvis ST, Oculus Optikgeräte GmbH; Wetzlar, Germany)
uses an ultra-high speed Scheimpflug camera that visualizes corneal changes
during deformation to produce various parameters [10]. The Pentacam HR topography and Corvis ST biomechanical
parameters were then analysed together using different artificial intelligence
methods [11]. A tomographic and biomechanical index
may provide greater accuracy for detecting subclinical keratoconus among eyes
clinically deemed to have ‘normal topography’ [11]. High-resolution
swept-source optical coherence tomography (SS-OCT) provides anterior segment
imaging and measurements in a single platform [12]. Newer
OCT platforms capture corneal topography and tomography, anterior segment
metrics, axial length measurement, and IOL calculation—Fig. 1 [13]. With OCT biometry, the ocular
measurement can be combined with high-resolution macular scans for simultaneous
screening for macular pathology [14]. In
addition, corneal epithelial thickness measurements may have a role in planning
for refractive surgery; or identification of early keratoconus through
identification of focal epithelial thinning usually associated with areas of
corneal steepening [15].
Fig.
1: High-resolution sweptsource optical coherence tomography imaging of the
anterior segment of a pseudophakic eye.
Wavefront
Aberrometry
The development of new instrumentation to measure human optical aberrations and the recent refinements in the excimer laser delivery systems have opened a new era in vision correction: patient-customized, wavefront-guided treatment. Modern aberrometers are equipped with a corneal topographer system to compute the effect of the anterior and posterior corneal contribution to the ocular wavefront, and by subtraction, the effect of internal optics (the crystalline lens, or an IOL in pseudophakia). As described later, aberrometry data can be used to generate custom wavefrontguided ablation profiles procedures that aim to correct both the spherocylindrical refraction and higher-order aberrations (HOAs). Wavefront aberrometers measure only monochromatic aberrations whereas our eyes can see a polychromatic world. In the future, the discrepancy between the measured monochromatic wavefront and the actual polychromatic wavefront may help to find the precise amount of HOAs to correct. The ideal flat wavefront for high fidelity may be optimal for young patients with intact accommodative abilities, whereas adjusted-shape designed to increase the depth of focus may be preferable for some presbyopic patients [17]. The functional needs of the patient will have to be taken into consideration to truly optimize wavefront refractive surgical strategies, and adaptative optic capabilities will certainly have to be accessible to achieve these tasks [18]. A new aberration series has been proposed to better fit the low- and higher-order components of the wavefront. This new basis may quantify the aberrations more accurately and provide clinicians with coefficient magnitudes which better underline the impact of clinically significant aberration modes [19].
Keratorefractive
surgery
Keratorefractive essentially involves treating refractive errors by reshaping the cornea—traditionally with an excimer laser, but now possible using only a femtosecond laser via refractive lenticule extraction [32]. The evolution of keratorefractive surgery began with surface ablation techniques such as photorefractive keratectomy (PRK) that involves epithelial removal [33],or laser epithelial keratomileusis (LASEK) where 20% alcohol is used to displace the corneal epithelium [34]. The detached epithelial sheet was initially preserved to reduce inflammation and pain, but later techniques involved removal as the alcohol was found to affect its vitality [35]. More recently, excimer laser ablation has been used to remove the corneal epithelium directly i.e. trans-epithelial PRK [36]. One advantage of trans-epithelial PRK is that the epithelial layer removal and excimer is performed at the same time—although most reports suggest that healing time and visual outcomes results do not vary greatly amongst various techniques of epithelium removal [37, 38]. Surface ablation has regained popularity over the past few years due to the safety of the surgery and better biomechanics [39], especially in patients with high myopia and thin corneas [40, 41]. While the refractive predictability of surface ablation is comparable with LASIK, myopic regression may be more common after surface ablation [42]. Moreover, scarring and haze can occur from the healing response in the Bowman’s layer and anterior corneal stroma [43]. Low-dose topical mitomycin- C (0.02–0.04%) is usually applied after excimer laser to reduce haze formation [44, 45]. Nonetheless, patients may still experience more discomfort after surface ablation compared with LASIK, due to the healing of the epithelium [46].
Laser
in situ keratomileusis (LASIK)
While LASIK corneal flaps were
previously created using an oscillating microkeratome [47], the addition of femtosecond lasers greatly reduced the risk of
some of the more significant flap complications such as buttonhole, free cap, and
irregular cuts [48]. One of the other main benefits of femtosecond
lasers was the improved reproducibility of flap thickness, which enabled the
use of thinner flaps with increased safety. Flap thickness reproducibility is
an important factor for residual stromal thickness (RST) safety planning as a
thicker than intended flap can lead to a lower than predicted RST and risk of
ectasia. The standard deviation of central flap thickness from older
microkeratomes was reported to be in the range of 20–40 μm [47, 49], compared with current femtosecond flap
thickness reproducibility of less than 5 μm [50, 51]. A review of LASIK outcomes was reported on by Sandoval et al. [4] in 2016. The authors reviewed articles published between 2008 and
2015 representing more than 67,000 eyes. They found UDVA was 20/40 or better in
99.5% of eyes, spherical equivalent refraction was within ±1 diopter (D) of target
in 98.6% of eyes, and loss of 2 or more lines of corrected distance visual
acuity (CDVA) was 0.61%. Subjectively, patients were very satisfied with only 1.2%
of patients reporting to be dissatisfied with the procedure. Within this
analysis were treatments that were performed as far back as 2008. Therefore,
some of the lasers that contributed to these outcomes would no longer fall into
the “modern laser” category in 2020, so we can only expect future reviews to
show even better outcomes. Despite these excellent outcomes, it is still
important to counsel patients on the occasional suboptimal effects, such as increased
glare and haloes, residual refractive error or irregular astigmatism [52]. Dry eye is one of the most common side effects, which is
usually temporary and may be managed with topical lubricants in most cases [53]. Postoperative flaprelated complications include flap
displacement, diffuse lamellar keratitis (DLK) [54], or
epithelial ingrowth [55], all of which may be treated with
topical eye drops or in some cases may require laser treatment or flap-lift [56]. Rarely, corneal ectasia can still occur, which has greatly
reduced with the advent of more accurate preoperative imaging and assessments
as already described [57]. Advances in excimer laser and
wavefront-guided treatments Both LASIK and surface ablation techniques rely on
the excimer laser to reshape the cornea, which were initially based on a
spherical shape as in the Munnerlyn formula. Aspheric profiles were first
tested by Seiler et al. [58] who demonstrated significantly less
induction of spherical aberration and glare. The introduction of flying spot
lasers and a Gaussian beam profile further improved outcomes. Laser frequency
has also been increasing over the years, which has reduced ablation time and
the impact of corneal dehydration. O’Brart et al. [59] showed that increasing optical zone diameter decreased the
impact of night vision disturbances, so modern lasers use large optical zones
and improved transition zones [60]. As described above, another advance
was the use of aberrometry measurements to treat naturally occurring HOAs [61–63]. However, wavefront-guided treatments did not eliminate residual HOAs,
but did slightly reduce the induction of spherical aberration [64]. Wavefront-optimized
treatments shifted the aim of the treatment to the control of spherical
aberration, but can have variable effects on other HOAs [65, 66]. An alternative method for custom
treatments is corneal
topography-guided laser ablation
[67], most useful where the refractive
error of the eye matches its corneal topography i.e. most of the aberration is
produced by the cornea [68]. Currently, excimer lasers with
active eye tracking systems to compensate for cyclotorsion and microsaccadic
eye movements are already considered common standards of care for such
treatments [69]. Beyond 2020: keratorefractive surgery
for presbyopia correction Traditionally, the principles used for monovision
have been applied to keratorefractive surgery [70, 71], to provide patients with good distance and reading vision with
high patient satisfaction [70, 72]. However,
careful patient selection is required, with the loss of fusion and stereoacuity
leading to poor acceptance as a potential outcome [73, 74]. Another option of keratorefractive
surgery for presbyopia correction is to create a ‘multifocal cornea’. The
majority of corneal multifocal treatments essentially creates a “central
island” to provide near vision, while a hybrid combination of multifocality
with some induced anisometropia may have improved safety [75, 76]. However, some studies using this
hybrid protocol report an unacceptable rate of loss of two lines of CDVA [77]. Therefore, caution must be used when treating the cornea with
any multifocal laser ablation profile because the change in optical quality can
increase the risk of losing lines of CDVA in poorly selected candidates.
Suggested selection criteria include low hyperopia (up to +3 D) or myopia (up
to −4 D), low astigmatism, a maximum requirement of +2 near vision add and photopic
pupillometry of less than 3.5 mm [78].
Recently, the application of extended depth of field in keratorefractive
surgery has come from the research on the use of spherical aberration to
increase the depth of field [79, 80]. Laser
blended vision (LBV) is based on nonlinear changes in asphericity. LBV is
tolerated by more than 95% of patients [81–83], compared with monovision which is tolerated by only between 59
and 67% of patients [84]. Because it is not a multifocal
treatment, LBV has also been shown to provide good distance, intermediate, and
near vision without the increased risk for losing lines of corrected visual
acuity [81, 82, 85].
Small
incision lenticule extraction (SMILE)
Following the introduction of the
VisuMax femtosecond laser (Carl Zeiss Meditec, Jena, Germany), an all
femtosecond laser, keyhole, flapless procedure was developed, referred to as
SMILE. The SMILE procedure involves using a femtosecond laser to delineate a
refractive lenticule within the stroma connected to the surface by a small
incision— Figs. 2. The femtosecond interfaces are
surgically separated and the refractive lenticule is removed through the small
incision. SMILE brings two main
advantages over LASIK: faster dry eye symptom recovery and better spherical
aberration control [86–88]. Both of
these advantages stem from the minimally invasive pocket incision that results
in maximal retention of anterior corneal innervation as well as structural
integrity. The evidence for reduced dry eye is supported by studies on corneal
nerve regeneration [89], and recovery of corneal sensitivity [90]. Biomechanically, SMILE offers a theoretical advantage over
LASIK by preservation of the stronger anterior stromal lamellae. Randleman et
al. [91] and Scarcelli et al. [92] demonstrated that the strength of the stroma decreases from
anterior to posterior within the central corneal region. Petsche et al. [93] found a similar result for transverse shear strength to decrease
with
 |
Fig. 2: Series of diagrams showing the femtosecond cutting sequence for a SMILE procedure. |
stromal depth. Applying this knowledge
to SMILE, since the anterior stroma remains uncut, the strongest part of the
stroma continues to contribute to the strength of the cornea postoperatively.
This has been evaluated using a
theoretical [94], finite element modeling [95, 96], and laboratory experiments [97]. The clinical effect is less induction of spherical aberration
compared with LASIK [98]. Therefore, it is possible to increase
the optical zone diameter with SMILE, further reducing the spherical aberration
induction, without compromising the corneal biomechanics compared with the equivalent
LASIK treatment [99].
Refinements
to SMILE
As SMILE has gained popularity, nearly
every aspect of the treatment has been optimized. Initially, the main weakness was
the slightly delayed visual recovery relative to the overnight ‘wow’ effect associated
with LASIK. However, detailed research into the energy level and spot/track
spacing has significantly improved visual recovery, without compromising the
ease of lenticule separation [100–104]. Most
published results suggest that SMILE is safe, effective, and predictable for
treating moderate myopia and modest levels of astigmatism [105], with postoperative visual outcomes comparable with femtosecond
LASIK [106, 107].
Vision-related quality of life has also been found to be comparable between
SMILE and LASIK [108–110]. Suction
loss is the most common complication for SMILE, with an incidence of about
0.50% [111–113]. However,
there is a clear management protocol for this, further guided by a decision
tree by Reinstein et al. [111, 112]. Thus, it
is possible to complete the treatment on the same day (continuing with SMILE or
converting to LASIK) without affecting the visual or refractive outcome [111, 112]. Postoperative complications of SMILE
are essentially the same as LASIK, however there are two areas where some small
differences have been identified. The first is with DLK where a unique appearing sterile multifocal inflammatory
keratitis can present after SMILE, which needs to be aggressively treated [114]. The second area is epithelial ingrowth, which can be more common due
to the instrument implanting epithelial cells within the interface by the
instruments through the small 2-mm incision. This can be successfully treated
by using a Nd:YAG laser or washing out the interface. Finally, a number of
options for retreatment or enhancement after SMILE have been developed, including
surface ablation, converting the cap in to a flap via side cut or Circle [115], and thin flap LASIK [116]. SMILE is
now a mature and established procedure [117] that
provides patients with a safe and effective outcome with current reports
demonstrating that the visual and refractive outcomes are similar to LASIK [87, 118–120].
Stromal
lenticule implantation
The increasing popularity of SMILE is
providing surgeons with thousands of human donor stromal lenticules that could
potentially be used for the treatment of presbyopia [7, 121], hyperopia [9, 122, 123], and
corneal ectatic diseases, such as keratoconus [124, 125]. The greater
precision of the femtosecond laser allow for more accurate stromal lenticule
creation, and may offer advantages over
commercialized synthetic inlays in the aspect of biocompatibility, retaining
nutrient flow within the stroma and reduced risk of extrusion. On the other
hand, these biological inlays have a low but potential risk for rejection, while
subject to eye banking and corneal transplantation regulations for donor
quality and safety. The preoperative decellularization of these donor
lenticules may reduce the risk of rejection [4, 124, 126, 127]. Preliminary
human clinical results suggest biocompatibility, safety and long-term
transparency of these implants in vivo [121–125]. However, one of the main limitations is the unpredictability of
the refractive outcome, which is dependent on the stromal remodeling of both
the inlay and the recipient stroma, leading to significant undercorrections [6, 123, 128, 129]. Further studies with larger samples, longer follow-ups,
technique refinements, and treatment nomograms are required. On the other hand,
encouraging results are being reported for advanced keratoconus, where a
precise refractive outcome is not the target, but refractive stability may
delay the need for corneal transplantation (Fig. 3) [124, 125]. Stromal lenticules (either plano or negative
meniscus shape) and allogenic stromal ring segments have been used in clinical
trials for keratoconus showing a moderate improvement in all visual, refractive
and keratometric parameters [31, 37, 38].
Fig.
3: Corneal stroma enhancement with a decellularized corneal stroma lenticule in
a patient with advanced keratoconus.
Intracorneal
implants
In 1949, José Ignacio Barraquer,
described the “thickness law”, forming the basis for intracorneal implants
leading to a hyperopic or myopic shift [130].
Keratophakia was described in 1964 as a lamellar refractive surgery procedure for
the treatment of hyperopia and presbyopia, but abandoned due to interface
scarring and unpredictable refractive results [131]. However,
this led to the development of synthetic
intracorneal implants known today as “inlays”. Early corneal inlays
(made of polymethyl-methacrylate- PMMA or polysulfone) were associated with
loss of transparency, corneal thinning or melting, and implant extrusion due to
interruption of nutrient flow within the stroma [132]. This critical
limitation was partially overcome with the development of intracorneal ring segments (ICRS), new synthetic inlays
with perforated designs, and new hydrogel biomaterials permitting the exchange
of nutrients, such as glucose and oxygen within the corneal stroma [132]. Today, intracorneal implants for the treatment of myopia and astigmatism
have been superseded by keratorefractive surgery. Intracorneal rings are made of inert, biocompatible synthetic
materials that are implanted deep into the stroma to modify the corneal
curvature and regularize its shape to reduce the refractive error—Fig. 4 [136]. Their capability to flatten the
central cornea, reduce keratometric values, and corneal astigmatism, have made ICRS
an important therapeutic approach for the visual rehabilitation of keratoconic
eyes. However, the low refractive predictability and significant risk of losing
corrected vision have caused ICRS to be abandoned as a purely refractive option
in non-pathologic eyes [137].
Fig.
4: Slit-lamp photograph of an eye with intracorneal implants. Intracorneal ring
implanted in a patient with keratoconus.
Presbyopia
corneal inlays
Corneal inlays have several theoretical
advantages: there is no corneal tissue removal, it is minimally invasive, and
can be explanted [138]. There are three types of corneal inlays
[138]: corneal
reshaping inlays to reshape of the anterior corneal curvature, leaving
a multifocal cornea; refractive
inlays where there is a modification on the refractive index of the
cornea with a bifocal optic; and small
aperture inlay which improves the depth of focus. Presbyopia inlays are
implanted in the nondominant eye, centered on the first Purkinje reflex within
a corneal pocket or under a stromal flap [133]. The implantation
depth depends on the inlay: those that alter the curvature of the cornea are
implanted more superficially, while those with a small aperture or a different
refraction index are implanted deeper to reduce anterior corneal curvature changes
and to allow a proper diffusion of nutrients within the corneal stroma [133]. The RaindropTM (ReVision
Optics Inc., Lake Forest, CA, USA) corneal
reshaping inlay is made of a biocompatible hydrogel material with 80%
water to allow the passage of nutrients within the corneal stroma (Fig. 5 left) [138]. It has no refractive power, formed by
smoothly transitioning regions that provide near vision in the steepest central
area, intermediate vision around this central area, and distance vision in the
periphery that is marginally affected by the inlay [138]. Despite most patients being satisfied, 7.8% of eyes required
inlay removal due to discontent with the visual outcome. Other complications
included marked glare (2.1%) or halos (4.1%) even one year after surgery; flap-related
dry eye syndrome (4.7%), and inlay-related central corneal haze (14%)—Fig. 5 right. The Raindrop implant was discontinued from the market in
January 2018 due to the evidence of late haze with loss of CDVA in clinical
practice [132]. The Flexivue MicrolensTM (Presbia Cooperatief U.A., Amsterdam,
Netherlands) and IcolensTM (Neoptics AG, Huenenberg, Switzerland) are bifocal inlays with a central
0.15 mm opening to facilitate the transfer of nutrients and oxygen through the
cornea, implanted into a corneal pocket at 280–300 µm depth in the nondominant
eye [133].
Fig.
5: Raindrop inlay. Slit lamp (left; white arrows point the edges of the inlay)
and anterior segment optical coherence tomography (OCT) pictures (right).
Light rays passing through the central
zone of the inlay that does not have refractive power will be sharply focused
for distance vision, while the refractive peripheral zone focus light rays on
the retina for near vision [133]. Available scientific evidence with
these inlays is far more limited, with monocular reduction of UDVA, loss of
contrast sensitivity and a significant frequent loss of CDVA reported [4, 16–18]. The Kamra VisionTM (Acufocus Inc.,
Irvine, CA, USA) is the most widely used corneal inlay, with nearly 20,000
inlays implanted worldwide [139]. It has a central 1.6 mm aperture, and
8400 microperforations (5–11 µm in diameter) in the peripheral opaque ring to
allow nutritional flow through the cornea (Fig. 6 left) [138]. However, as it is an opaque inlay it may be very obvious in
light-colored eyes. It improves near vision by increasing the depth of focus
through the principle of small aperture optics (blockage of the peripheral
unfocused rays of light) [139]. It is usually implanted into a 6 × 6
mm diameter stomal pocket and 200–270 µm depth in the nondominant eye. A
prospective, multicenter clinical trial (507 eyes with emmetropic presbyopia
and 3-year follow-up) reported an average 3.3-line improvement in UNVA, 1-line
improvement in UIVA, and 0.4-line reduction in UDVA on the implanted eye, while
no loss in binocular distance vision was observed [19]. Despite the opaque nature of this inlay, no scotomas in the
visual field have been observed, with a mean reduction of ~1 dB in contrast
sensitivity [138]. 8.7% of eyes required inlay removal
due to dissatisfaction with the visual outcome. Other complications included significant
glare (19%), halos (25%) night vision problems (30%), and inlay-related central
corneal haze (2.8%)—Fig. 6, middle.
Future
of intracorneal implants and corneal inlays
Corneal inlays have proven to be an
effective alternative for presbyopia management. However, the future of inlays
beyond 2020 looks uncertain. Despite clinical investigation for more than 15
years, they have still not gained full popularity among refractive surgeons due
to the frequent problems of centration, biological intolerance, and optical
performance, causing a relatively high explantation rate over time secondary to
late complications such as corneal stromal opacities, late hyperopic shift or
inadequate visual performance [26]. The most promising of inlays remain
the Kamra implant where it was observed in that UNVA, refractive stability,
patient satisfaction, haze risk, and explantation rate significantly improved
when the Kamra was implanted inside a lamellar pocket (and not a flap). This
stromal pocket was created with a femtosecond laser using tight spot-line
separation settings and with a depth ≥40% of the total corneal thickness. This
could be due to a reduction in wound-healing response due to the reduced
keratocyte density of the posterior stroma [19]. Similar
outcomes were previously reported by other authors including eyes with previous
cataract surgery with a monofocal IOL [21–23]. Perhaps more importantly, it has been shown that the procedure
is reversible—Alió et al. demonstrated that Kamra inlay removal can be safely
performed without permanently affecting corneal topography and aberrometry,
with more than 60% of patients recovered preoperative visual acuity [24]. Certainly, more improvements are needed in the future as
careful slit-lamp examination showed in most cases a mild haze, and
occasionally, prominent donutlike scarring (Fig. 6 right) [24]. Corneal confocal microscopy demonstrated that the Kamra inlay
had good intrastromal tolerance, although a low grade of keratocyte activation
was found in all patients, and a stronger response was associated with a
negative visual outcome [25].
Fig. 6 Kamra inlay. Slit-lamp pictures 3 months (left; observe the peripheral
microperforations to allow corneal nutrition) and 3 years after implantation
(middle). Note the progressive moderate haze associated with visual loss that
justified inlay explantation, remaining a donut-shape central corneal scar
still visible 4 years after inlay removal (right).
References
1. Kim
TI, Alio Del Barrio JL, Wilkins M, Cochener B, Ang M. Refractive surgery.
Lancet. 2019;393:2085–98.
2. Sugar
A, Hood CT, Mian SI. Patient-reported outcomes following LASIK: quality of Life
in the PROWL Studies. JAMA. 2017;317:204–5.
3. Sugar
A, Rapuano CJ, Culbertson WW, Huang D, Varley GA, Agapitos PJ, et al. Laser in
situ keratomileusis for myopia and astigmatism: safety and efficacy: a report
by the American Academy of Ophthalmology. Ophthalmology. 2002;109:175–87.
4. Sandoval
HP, Donnenfeld ED, Kohnen T, Lindstrom RL, Potvin R, Tremblay DM, et al. Modern
laser in situ keratomileusis outcomes. J Cataract Refract Surg.
2016;42:1224–34.
5. Eydelman
M, Hilmantel G, Tarver ME, Hofmeister EM, May J, Hammel K, et al. Symptoms and satisfaction
of patients in the patient-reported outcomes with laser in situ keratomileusis (PROWL)
studies. JAMA Ophthalmol. 2017;135:13–22.
6. Ang
M, Mehta JS, Chan C, Htoon HM, Koh JC, Tan DT. Refractive lenticule extraction:
transition and comparison of 3 surgical techniques. J Cataract Refract Surg.
2014;40:1415–24.
7. Ang
M, Tan D, Mehta JS. Small incision lenticule extraction (SMILE) versus laser
in-situ keratomileusis (LASIK): study protocol for a randomized,
non-inferiority trial. Trials. 2012;13:75.
8. Mi
H, Tan N, Ang M, Htoon HM, Mehta JS. Comparison of anterior and posterior
topographic analysis between 3 imaging systems. J Cataract Refract Surg. 2015;41:2533–45.
9. Chan
C, Ang M, Saad A, Chua D, Mejia M, Lim L, et al. Validation of an objective
scoring system for forme fruste keratoconus detection and post-LASIK ectasia
risk assessment in Asian eyes. Cornea. 2015;34:996–1004.
10. Roberts
CJ, Mahmoud AM, Bons JP, Hossain A, Elsheikh A, Vinciguerra R, et al.
Introduction of two novel stiffness parameters and interpretation of air puff-induced
biomechanical deformation parameters with a dynamic Scheimpflug analyzer. J Refract
Surg. 2017;33:266–73.
11. Ambrosio
R Jr., Lopes BT, Faria-Correia F, Salomao MQ, Buhren J, Roberts CJ, et al.
Integration of Scheimpflug-based corneal tomography and biomechanical
assessments for enhancing ectasia detection. J Refract Surg. 2017;33:434–43.
12. Ang
M, Baskaran M, Werkmeister RM, Chua J, Schmidl D, Aranha Dos Santos V, et al.
Anterior segment optical coherence tomography. Prog Retin Eye Res. 2018;66:132 56.
13. Ang
M, Chong W, Huang H, Tay WT, Wong TY, He MG, et al. Comparison of anterior
segment optical tomography parameters measured using a semi-automatic software
to standard clinical instruments. PLoS ONE. 2013;8:e65559.
14. Sikorski
BL, Suchon P. OCT biometry (B-OCT): a new method for measuring ocular axial
dimensions. J Ophthalmol. 2019;2019:9192456.
15. Silverman
RH, Urs R, Roychoudhury A, Archer TJ, Gobbe M, Reinstein DZ. Epithelial remodeling
as basis for machine-based identification of keratoconus. Investig Ophthalmol
Vis Sci. 2014;55:1580–7
16. Gatinel
D, Azar DT, Dumas L, Malet J. Effect of anterior corneal surface asphericity
modification on fourth-order zernike spherical aberrations. J Refract Surg.
2014;30:708–15.
17. Amigo
A, Martinez-Sorribes P, Recuerda M. Refractive changes induced by spherical
aberration in laser correction procedures: an adaptive optics study. J Refract Surg.
2017;33:470–4.
18. Gatinel
D, Malet J, Dumas L. Polynomial decomposition method for ocular wavefront
analysis. J Opt Soc Am A Opt Image Sci Vis. 2018;35:2035–45.
19. Artal
P, Benito A, Perez GM, Alcon E, De Casas A, Pujol J, et al. An objective
scatter index based on double-pass retinal images of a point source to classify
cataracts. PLoS ONE. 2011;6:e16823.
20. Panthier
C, de Wazieres A, Rouger H, Moran S, Saad A, Gatinel D. Average lens density
quantification with swept-source optical coherence tomography: optimized,
automated cataract grading technique. J Cataract Refract Surg. 2019;45:1746–52.
21. Accardo
PA, Pensiero S. Neural network-based system for early keratoconus detection
from corneal topography. J Biomed Inf. 2002;35:151–9.
22. Kovacs
I, Mihaltz K, Kranitz K, Juhasz E, Takacs A, Dienes L, et al. Accuracy of
machine learning classifiers using bilateral data from a Scheimpflug camera for
identifying eyes with preclinical signs of keratoconus. J Cataract Refract
Surg. 2016;42:275–83.
23. Arbelaez
MC, Versaci F, Vestri G, Barboni P, Savini G. Use of a support vector machine
for keratoconus and subclinical keratoconus detection by topographic and tomographic
data. Ophthalmology. 2012;119:2231–8.
24. Smadja
D, Touboul D, Cohen A, Doveh E, Santhiago MR, Mello GR, et al. Detection of
subclinical keratoconus using an automated decision tree classification. Am J
Ophthalmol. 2013;156:237–46 e231.
25. Connell
BJ, Kane JX. Comparison of the Kane formula with existing formulas for
intraocular lens power selection. BMJ Open Ophthalmol. 2019;4:e000251.
26. Kanellopoulos
AJ, Pallikaris IG, Donnenfeld ED, Detorakis S, Koufala K, Perry HD. Comparison
of corneal sensation following photorefractive keratectomy and laser in situ
keratomileusis. J Cataract Refract Surg. 1997;23:34–8.
27. Amm
M, Wetzel W, Winter M, Uthoff D, Duncker GI. Histopathological comparison of photorefractive
keratectomy and laser in situ keratomileusis in rabbits. J Refract
Surg.1996;12:758–66.
28. Azar
DT, Ang RT, Lee JB, Kato T, Chen CC, Jain S, et al. Laser subepithelial
keratomileusis: electron microscopy and visual outcomes of flap photorefractive
keratectomy. Curr Opin Ophthalmol. 2001;12:323–8.
29. Chen
CC, Chang JH, Lee JB, Javier J, Azar DT. Human corneal epithelial cell
viability and morphology after dilute alcohol exposure. Investig Ophthalmol Vis
Sci. 2002;43:2593–602.
30. Fadlallah
A, Fahed D, Khalil K, Dunia I, Menassa J, El Rami H, et al. Transepithelial
photorefractive keratectomy: clinical results. J Cataract Refract Surg.
2011;37:1852–7.
31. Antonios
R, Abdul Fattah M, Arba Mosquera S, Abiad BH, Sleiman K, Awwad ST. Single-step
transepithelial versus alcohol-assisted photorefractive keratectomy in the
treatment of high myopia: a comparative evaluation over 12 months. Br J Ophthalmol.
2017;101:1106–12.
32. Wen
D, McAlinden C, Flitcroft I, Tu R, Wang Q, Alio J, et al. Postoperative
efficacy, predictability, safety, and visual quality of laser corneal
refractive surgery: a network meta-analysis. Am J Ophthalmol. 2017;178:65–78.
33. Sanchez
P, Moutsouris K, Pandolfi A. Biomechanical and optical behavior of human
corneas before and after photorefractive keratectomy. J Cataract Refract Surg. 2014;40:905–17.
34. Vestergaard
AH. Past and present of corneal refractive surgery: a retrospective study of
long-term results after photorefractive keratectomy and a prospective study of
refractive lenticule extraction. Acta Ophthalmol. 2014;2:1–21. 92
35. Munnerlyn
CR, Koons SJ, Marshall J. Photorefractive keratectomy: a technique for laser
refractive surgery. J Cataract Refract Surg. 1988;14:46–52.
36. Na
KS, Chung SH, Kim JK, Jang EJ, Lee NR, Joo CK. Comparison of LASIK and surface
ablation by using propensity score analysis: a multicenter study in Korea.
Investig Ophthalmol Vis Sci. 2012;53:7116–21.
37. Wachtlin
J, Langenbeck K, Schrunder S, Zhang EP, Hoffmann F. Immunohistology of corneal
wound healing after photorefractive keratectomy and laser in situ
keratomileusis. J Refract Surg. 1999;15:451–8.
38. Kim
TI, Pak JH, Lee SY, Tchah H. Mitomycin C-induced reduction of keratocytes and
fibroblasts after photorefractive keratectomy. Investig Ophthalmol Vis Sci.
2004;45:2978–84.
39. Lee
DH, Chung HS, Jeon YC, Boo SD, Yoon YD, Kim JG. Photorefractive keratectomy with
intraoperative mitomycin-C application. J Cataract Refract Surg.
2005;31:2293–8.
40. Faktorovich
EG, Melwani K. Efficacy and safety of pain relief medications after
photorefractive keratectomy: review of prospective randomized trials. J
Cataract Refract Surg. 2014;40:1716–30.
41. Shemesh
G, Dotan G, Lipshitz I. Predictability of corneal flap thickness in laser in
situ keratomileusis using three different microkeratomes. J Refract Sur.
2002;18:S347–351.
42. Santhiago
MR, Kara-Junior N, Waring GOt. Microkeratome versus femtosecond flaps: accuracy
and complications. Curr Opin Ophthalmol. 2014;25:270–4.
43. Solomon
KD, Donnenfeld E, Sandoval HP, Al Sarraf O, Kasper TJ, Holzer MP, et al. Flap
thickness accuracy: comparison of 6 microkeratome models. J Cataract Refract
Surg. 2004;30:964–77.
44. Reinstein
DZ, Archer TJ, Gobbe M. Accuracy and reproducibility of Cap thickness in small
incision lenticule extraction. J Refract Surg. 2013;29:810–5.
45. Zhai
CB, Tian L, Zhou YH, Zhang QW, Zhang J. Comparison of the flaps made by
femtosecond laser and automated keratomes for sub-bowman keratomileusis. Chin
Med J. 2013;126:2440–4.
46. Zhao
LQ, Wei RL, Cheng JW, Li Y, Cai JP, Ma XY. Metaanalysis: clinical outcomes of
laser-assisted subepithelial keratectomy and photorefractive keratectomy in
myopia. Ophthalmology. 2010;117:1912–22.
47. Wallerstein
A, Jackson WB, Chambers J, Moezzi AM, Lin H, Simmons PA. Management of post-LASIK
dry eye: a multicenter randomized comparison of a new multi-ingredient artificial
tear to carboxymethylcellulose. Clin Ophthalmol. 2018;12:839 48.
48. Segev
F, Mimouni M, Sela T, Munzer G, Kaiserman I. Risk factors for sporadic diffuse
lamellar keratitis after microkeratome laser-assisted in situ keratomileusis: a
retrospective large database analysis. Cornea. 2018;37:1124–9.
49. Yesilirmak
N, Chhadva P, Cabot F, Galor A, Yoo SH. Post-laser in situ keratomileusis
epithelial ingrowth: treatment, recurrence, and long-term results. Cornea.
2018;37:1517–21.
50. Ayala
MJ, Alio JL, Mulet ME, De La Hoz F. Treatment of laser in situ keratomileusis
interface epithelial ingrowth with neodymium: yytrium-aluminum-garnet laser. Am
J Ophthalmol. 2008;145:630–4.
51. Bohac
M, Koncarevic M, Pasalic A, Biscevic A, Merlak M, Gabric N, et al. Incidence
and clinical characteristics of post LASIK ectasia: a review of over 30,000
LASIK cases. Semin Ophthalmol. 2018;33:869–77.
52. Seiler
T, Genth U, Holschbach A, Derse M. Aspheric photorefractive keratectomy with
excimer laser. Refract Corneal Surg. 1993;9:166–72.
53. O’Brart
DP, Corbett MC, Lohmann CP, Kerr Muir MG, Marshall J. The effects of ablation
diameter on the outcome of excimer laser photorefractive keratectomy. A
prospective, randomized, double-blind study.
Arch Ophthalmol. 1995;113:438–43.
54. Kalski
RS, Sutton G, Bin Y, Lawless MA, Rogers C. Comparison of 5-mm and 6-mm ablation
zones in photorefractive keratectomy for myopia. J Refract Surg. 1996;12:61–7.
55. Buhren
J, Pesudovs K, Martin T, Strenger A, Yoon G, Kohnen T. Comparison of optical
quality metrics to predict subjective quality of vision after laser in situ
keratomileusis. J Cataract Refract Surg. 2009;35:846–5.
56. Drum
BA. Aberration analyses needed for FDA evaluation of safety and effectiveness
of wavefront-guided refractive surgical devices. J Refract Surg.
2003;19:S588–91.
57. Pesudovs
K. Wavefront aberration outcomes of LASIK for high myopia and high hyperopia. J
Refract Surg. 2005;21:S508–12.
58. Myrowitz
EH, Chuck RS. A comparison of wavefront-optimized and wavefront-guided ablations.
Curr Opin Ophthalmol. 2009;20:247–50.
59. Jun
I, Kang DS, Tan J, Choi JY, Heo W, Kim JY, et al. Comparison of clinical
outcomes between wavefront-optimized versus corneal wavefront-guided transepithelial
photorefractive keratectomy for myopic astigmatism. J Cataract Refract
Surg.2017;43:174–82.
60. Lee
WS, Manche EE. Comparison of simulated keratometric changes following wavefront-guided
and wavefront-optimized myopic laser-assisted in situ keratomileusis. Clin
Ophthalmol. 2018;12:613–9.
61. Moshirfar
M, Shah TJ, Skanchy DF, Linn SH, Kang P, Durrie DS. Comparison and analysis of
FDA reported visual outcomes of the three latest platforms for LASIK: wavefront
guided VisxiDesign, topography guided WaveLight Allegro Contoura, and topography
guided Nidek EC-5000 CATz. Clin Ophthalmol. 2017;11:135–47.
62. Schallhorn
SC, Farjo AA, Huang D, Boxer Wachler BS, Trattler WB, Tanzer DJ, et al.
Wavefront-guided LASIK for the correction of primary myopia and astigmatism a
report by the American Academy of Ophthalmology. Ophthalmology.
2008;115:1249–61.
63. Smadja
D, Reggiani-Mello G, Santhiago MR, Krueger RR. Wavefront ablation profiles in
refractive surgery: description, results, and limitations. J Refract Surg.
2012;28:224–32.
64. Goldberg
DB. Laser in situ keratomileusis monovision. J Cataract Refract Surg.
2001;27:1449–55.
65. Miranda
D, Krueger RR. Monovision laser in situ keratomileusis for pre-presbyopic and
presbyopic patients. J Refract Surg. 2004;20:325–8.
66. Ayoubi
MG, Leccisotti A, Goodall EA, McGilligan VE, Moore TC. Femtosecond laser in
situ keratomileusis versus conductive keratoplasty to obtain monovision in
patients with emmetropic presbyopia. J Cataract Refract Surg. 2010;36:997–1002.
67. Fawcett
SL, Herman WK, Alfieri CD, Castleberry KA, Parks MM, Birch EE. Stereoacuity and
foveal fusion in adults with long-standing surgical monovision. J Aapos.
2001;5:342–7.
68. Kato
S, Ito M, Shimizu K, Kamiya K. Etiology and outcomes of secondary surgical
intervention for dissatisfied patients after pseudophakic monovision. Int
Ophthalmol. 2018;38:1003–9.
69. Holland
D. PresbyLASIK treatment for simultaneous correction of presbyopia and ametropia:
development to PresbyMAX hybrid at the Augenklinik Bellevue. ESCRS. 2014.
70. Chan
TC, Kwok PS, Jhanji V, Woo VC, Ng AL. Presbyopic correction using monocular
Bi-aspheric ablation profile (PresbyMAX) in hyperopic eyes: 1-year outcomes. J
Refract Surg. 2017;33:37–43.
71. Luger
MH, McAlinden C, Buckhurst PJ, Wolffsohn JS, Verma S, Arba Mosquera S.
Presbyopic LASIK using hybrid biaspheric micro-monovision ablation profile for
presbyopic corneal treatments. Am J Ophthalmol. 2015;160:493–505.
72. Vargas-Fragoso
V, Alio JL. Corneal compensation of presbyopia: PresbyLASIK: an updated review.
Eye Vis. 2017;4:11.
73. Rocha
KM, Vabre L, Chateau N, Krueger RR. Expanding depth of focus by modifying
higher-order aberrations induced by an adaptive optics visual simulator. J
Cataract Refract Surg. 2009;35:1885–92.
74. Benard
Y, Lopez-Gil N, Legras R. Optimizing the subjective depth-of-focus with
combinations of fourth- and sixth-order spherical aberration. Vis Res.
2011;51:2471–7.
75. Reinstein
DZ, Archer TJ, Gobbe M. Laser blended vision for presbyopia correction. In:
Pallikaris IG, Plainis S, Charman WN, (eds). Presbyopia: origins, effects and
treatment. Thorofare, NJ: SLACK Incorporated; 2012.
76. Reinstein
DZ, Archer TJ, Gobbe M. LASIK for myopic astigmatism and presbyopia using
non-linear aspheric micromonovision with the Carl Zeiss Meditec MEL 80
platform. J Refract Surg. 2011;27:23–37.
77. Reinstein
DZ, Couch DG, Archer TJ. LASIK for hyperopic astigmatism and presbyopia using
Micro-monovision With the Carl Zeiss Meditec MEL80. J Refract Surg.
2009;25:37–58.
78. Evans
BJ. Monovision: a review. Ophthalmic Physiol Opt. 2007;27:417–39.
79. Reinstein
DZ, Carp GI, Archer TJ, Gobbe M. LASIK for the correction of presbyopia in emmetropic
patients using aspheric ablation profiles and a micro-monovision protocol with
the Carl Zeiss Meditec MEL80 and VisuMax. J Refract Surg. 2012;28:531–41.
80. Vestergaard
AH, Grauslund J, Ivarsen AR, Hjortdal JO. Efficacy, safety, predictability,
contrast sensitivity, and aberrations after femtosecond laser lenticule
extraction. J Cataract Refract Surg. 2014;40:403–11.
81. Sekundo
W, Gertnere J, Bertelmann T, Solomatin I. One-year refractive results, contrast
sensitivity, high-order aberrations and complications after myopic small-incision
lenticule extraction (ReLEx SMILE). Graefes Arch Clin Exp Ophthalmol. 2014;252:837–43.
82. Moshirfar
M, McCaughey MV, Reinstein DZ, Shah R, Santiago- Caban L, Fenzl CR.
Small-incision lenticule extraction. J Cataract Refract Surg. 2015;41:652–65.
83. Denoyer
A, Landman E, Trinh L, Faure JF, Auclin F, Baudouin C. Dry eye disease after
refractive surgery: comparative outcomes of small incision lenticule extraction
versus LASIK. Ophthalmology. 2015;122:669–76.
84. Reinstein
DZ, Archer TJ, Gobbe M, Bartoli E. Corneal sensitivity after small-incision
lenticule extraction and laser in situ keratomileusis. J Cataract Refract Surg.
2015;41:1580–7.
85. Randleman
JB, Dawson DG, Grossniklaus HE, McCarey BE, Edelhauser HF. Depth-dependent
cohesive tensile strength in human donor corneas: implications for refractive
surgery. J Refract Surg. 2008;24:S85–9.
86. Scarcelli
G, Pineda R, Yun SH. Brillouin optical microscopy for corneal biomechanics.
Investig Ophthalmol Vis Sci. 2012;53:185–90.
87. Petsche
SJ, Chernyak D, Martiz J, Levenston ME, Pinsky PM. Depth-dependent transverse
shear properties of the human corneal stroma. Investig Ophthalmol Vis Sci.
2012;53: 873–80.
88. Reinstein
DZ, Archer TJ, Randleman JB. Mathematical model to compare the relative tensile
strength of the cornea after PRK, LASIK, and small incision lenticule
extraction. J Refract Surg. 2013;29:454–60.
89. Seven
I, Vahdati A, Pedersen IB, Vestergaard A, Hjortdal J, Roberts CJ, et al.
Contralateral eye comparison of SMILE and Flap-Based corneal refractive surgery:
computational analysis of biomechanical impact. J Refract Surg. 2017;33:444–53.
90. Sinha
Roy A, Dupps WJ Jr., Roberts CJ. Comparison of biomechanical effects of
small-incision lenticule extraction and laser in situ keratomileusis:
finite-element analysis. J Cataract Refract Surg. 2014;40:971–80.
91. Spiru
B, Kling S, Hafezi F, Sekundo W. Biomechanical differences between femtosecond lenticule
extraction (FLEx) and small incision lenticule extraction (SmILE) tested by 2Dextensometry
in ex vivo porcine eyes. Investig Ophthalmol Vis Sci. 2017;58:2591–5.
92. Pedersen
IB, Ivarsen A, Hjortdal J. Changes in astigmatism, densitometry, and aberrations
after SMILE for low to high myopic astigmatism: a 12-month prospective study. J
Refract Surg. 2017;33:11–7.
93. Damgaard
IB, Ang M, Mahmoud AM, Farook M, Roberts CJ, Mehta JS. Functional optical zone
and centration following SMILE and LASIK: a prospective, randomized,
contralateral Eye Study. J Refract Surg. 2019;35:230–7.
94. Han
T, Shang J, Zhou X, Xu Y, Ang M, Zhou X. Refractive outcomes comparing small-incision
lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis
for high myopia. J Cataract Refract Surg. 2020;46:419–27.
95. Ji
YW, Kang DSY, Reinstein DZ, Archer TJ, Choi JY, Kim EK, et al. Effect of lowering
laser energy on the surface roughness of human corneal lenticules in small-incision
lenticule extraction. J Refract Surg. 2017;33:617–24.
96. Ji
YW, Kim M, Yong Kang DS, Reinstein D, Archer T, Choi JY, et al. Lower laser
energy levels lead to better visual recovery after small-incision lenticule
extraction: prospective, randomized clinical trial. Am J Ophthalmol.
2017;179:159–70.
97. Donate
D, Thaeron R. Lower energy levels improve visual recovery in small incision
lenticule extraction (SMILE). J Refract Surg. 2016;32:636–42.
98. Li
L, Schallhorn JM, Ma J, Cui T, Wang Y. Energy setting and visual outcomes in
SMILE: a retrospective Cohort Study. J Refract Surg. 2018;34:11–6.
99. Shen
Z, Shi K, Yu Y, Yu X, Lin Y, Yao K. Small incision lenticule extraction (SMILE)
versus femtosecond laser-assisted in situ keratomileusis (FS-LASIK) for myopia:
a systematic review and meta-analysis. PLoS ONE. 2016;11:e0158176.
100.
Zhang Y, Shen Q, Jia Y,
Zhou D, Zhou J. Clinical outcomes of SMILE and FS-LASIK used to treat myopia: a
meta-analysis. J Refract Surg. 2016;32:256–65.
101.
Ang M, Farook M, Htoon
HM, Mehta JS. Randomized clinical trial comparing femtosecond LASIK and
small-incision lenticule extraction. Ophthalmology. 2020;127:724–30.
102.
Ang M, Ho H, Fenwick E,
Lamoureux E, Htoon HM, Koh J, et al. Vision-related quality of life and visual
outcomes after small-incision lenticule extraction and laser in situ
keratomileusis. J Cataract Refract Surg. 2015;41:2136–44.
103.
Ang M, Farook M, Htoon
HM, Tan D, Mehta JS. Simulated night vision after small-incision lenticule
extraction. J Cataract Refract Surg. 2016;42:1173–80.
104.
Damgaard IB, Ang M,
Farook M, Htoon HM, Mehta JS. Intraoperative patient experience and
postoperative visual quality after SMILE and LASIK in a randomized, paired-eye,
controlled study. J Refract Surg. 2018;34:92–9.
105.
Reinstein DZ, Archer
TJ, Vida RS, Carp GI. Suction stability management in small incision lenticule
extraction: incidence and outcomes of suction loss in 4000 consecutive
procedures. Acta Ophthalmol. 2020;98:e72–e80.
106.
Reinstein DZ, Archer
TJ, Vida RS, Carp GI. Suction stability in SMILE: development of a decision
tree for managing eye movements and suction loss. J Refract Surg. 2018;34:809–16.
107.
Ang M, Chaurasia SS,
Angunawela RI, Poh R, Riau A, Tan D, et al. Femtosecond lenticule extraction
(FLEx): clinical results, interface evaluation, and intraocular pressure
variation. Investig Ophthalmol Vis Sci. 2012;53:1414–21.
108.
Reinstein DZ, Stuart
AJ, Vida RS, Archer TJ, Carp GI. Incidence and outcomes of sterile multifocal
inflammatory keratitis and diffuse lamellar keratitis after SMILE. J Refract
Surg. 2018;34:751–9.
109.
Siedlecki J, Luft N,
Mayer WJ, Siedlecki M, Kook D, Meyer B, et al. CIRCLE enhancement after myopic
SMILE. J Refract Surg. 2018;34:304–9.
110.
Reinstein DZ, Carp GI,
Archer TJ, Vida RS. Outcomes of retreatment by LASIK After SMILE. J Refract
Surg. 2018;34:578–88.
111.
Reinstein DZ, Archer
TJ, Carp GI. The surgeon’s guide to small incision lenticule extraction (SMILE).
Thorofare, New Jersey: SLACK Incorporated; 2018.
112.
Ganesh S, Gupta R.
Comparison of visual and refractive outcomes following femtosecond laser-
assisted lasik with smile in patients with myopia or myopic astigmatism. J
Refract Surg. 2014;30:590–6.
113.
Reinstein DZ, Carp GI,
Archer TJ, Gobbe M. Outcomes of small incision lenticule extraction (SMILE) in
low myopia. J Refract Surg. 2014;30:812–8.
114.
Pradhan KR, Reinstein DZ,
Carp GI, Archer TJ, Gobbe M, Dhungana P. Quality control outcomes analysis of
small-incision lenticule extraction for
myopia by a novice surgeon at the first refractive surgery unit in Nepal during
the first 2 years of operation. J Cataract Refract Surg. 2016;42:267–74.
115.
Jacob S, Kumar DA,
Agarwal A, Agarwal A, Aravind R, Saijimol AI. Preliminary evidence of
successful near vision enhancement with a new technique: PrEsbyopic Allogenic Refractive
Lenticule (PEARL) Corneal Inlay Using a SMILE Lenticule. J Refract Surg.
2017;33:224–9.
116.
Li M, Li M, Sun L, Ni
K, Zhou X. Predictive formula for refraction of autologous lenticule
implantation for hyperopia correction. J Refract Surg. 2017;33:827–33.
117.
Pradhan KR, Reinstein DZ,
Carp GI, Archer TJ, Gobbe M, Gurung R. Femtosecond laser-assisted keyhole
endokeratophakia: correction of hyperopia by implantation of an allogeneic lenticule
obtained by SMILE from a myopic donor. J Refractive Surg. 2013;29:777–82.
118.
Alio Del Barrio JL, El
Zarif M, Azaar A, Makdissy N, Khalil C, Harb W, et al. Corneal stroma enhancement
with decellularized stromal laminas with or without stem cell recellularization
for advanced keratoconus. Am J Ophthalmol. 2018;186:47–58.
119.
Mastropasqua L, Nubile
M, Salgari N, Mastropasqua R. Femtosecond laser-assisted stromal lenticule
addition keratoplasty for the treatment of advanced keratoconus: a Preliminary
Study. J Refract Surg. 2018;34:36–44.
120.
Alio del Barrio JL,
Chiesa M, Garagorri N, Garcia-Urquia N, Fernandez-Delgado J, Bataille L, et al.
Acellular human corneal matrix sheets seeded with human adipose-derived
mesenchymal stem cells integrate functionally in an experimental animal model.
Exp Eye Res. 2015;132:91–100.
121.
Liu YC, Teo EPW, Ang
HP, Seah XY, Lwin NC, Yam GHF, et al. Biological corneal inlay for presbyopia
derived from small incision lenticule extraction (SMILE). Sci Rep. 2018;8:1831.
122.
Liu R, Zhao J, Xu Y, Li
M, Niu L, Liu H, et al. Femtosecond laser-assisted corneal small incision allogenic
intrastromal lenticule implantation in monkeys: a Pilot Study. Investig
Ophthalmol Vis Sci. 2015;56:3715–20.
123.
Damgaard IB, Ivarsen A,
Hjortdal J. Biological lenticule implantation for correction of hyperopia: an
ex vivo study in human corneas. J Refract Surg. 2018;34:245–52.
124.
Barraquer JI.
Modification of refraction by means of intracorneal inclusions. Int Ophthalmol
Clin. 1966;6:53–78.
125.
Barraquer JI.
Keratophakia. Trans ophthalmological societies U Kingd. 1972;92:499–516.
126.
Garza EB, Gomez S,
Chayet A, Dishler J. One-year safety and efficacy results of a hydrogel inlay
to improve near vision in patients with emmetropic presbyopia. J Refract Surg. 2013;29:166–72.
127.
Malandrini A, Martone
G, Menabuoni L, Catanese AM, Tosi GM, Balestrazzi A, et al. Bifocal refractive
corneal inlay implantation to improve near vision in emmetropic presbyopic patients.
J Cataract Refract Surg. 2015;41:1962–72.
128.
Yilmaz OF, Bayraktar S,
Agca A, Yilmaz B, McDonald MB, vande Pol C. Intracorneal inlay for the surgical
correction of presbyopia. J Cataract Refract Surg. 2008;34:1921–7.
129.
Mulet ME, Alio JL,
Knorz MC. Hydrogel intracorneal inlays for the correction of hyperopia: outcomes
and complications after 5 years of follow-up. Ophthalmology. 2009;116:1455–60.
1460. e1451.
130.
Vega-Estrada A, Alio
JL. The use of intracorneal ring segments in keratoconus. Eye Vis. 2016;3:8.
131.
Vega-Estrada A, Alio
JL, Brenner LF, Javaloy J, Plaza Puche AB, Barraquer RI, et al. Outcome
analysis of intracorneal ring segments for the treatment of keratoconus based
on visual, refractive, and aberrometric impairment. Am J Ophthalmol. 2013;155:575–84.e571.
132.
Lindstrom RL, Macrae
SM, Pepose JS, Hoopes PC Sr. Corneal inlays for presbyopia correction. Curr
Opin Ophthalmol. 2013;24:281–7.
133.
Konstantopoulos A,
Mehta JS. Surgical compensation of presbyopia with corneal inlays. Expert Rev
Med Devices. 2015;12:341–52.
134.
Arlt E, Krall E, Moussa
S, Grabner G, Dexl A. Implantable inlay devices for presbyopia: the evidence to
date. Clin Ophthalmol. 2015;9:129–37.
135.
Whitman J, Dougherty
PJ, Parkhurst GD, Olkowski J, Slade SG, Hovanesian J, et al. Treatment of
presbyopia in emmetropes using a shape-changing corneal inlay: one-year
clinical outcomes. Ophthalmology. 2016;123:466–75.
136.
Yoo A, Kim JY, Kim MJ,
Tchah H. Hydrogel inlay for presbyopia: objective and subjective visual
outcomes. J Refract Surg. 2015;31:454–60.
137.
Limnopoulou AN,
Bouzoukis DI, Kymionis GD, Panagopoulou SI, Plainis S, Pallikaris AI, et al. Visual
outcomes and safety of a refractive corneal inlay for presbyopia using
femtosecond laser. J Refract Surg. 2013;29:12–8.
138.
Baily C, Kohnen T,
O’Keefe M. Preloaded refractive-addition corneal inlay to compensate for
presbyopia implanted using a femtosecond laser: one-year visual outcomes and
safety. J Cataract Refract Surg. 2014;40:1341–8.
139.
Vukich JA, Durrie DS,
Pepose JS, Thompson V, van de Pol C, Lin L. Evaluation of the small-aperture
intracorneal inlay: Three year results from the cohort of the U.S. Food and
Drug Administration clinical trial. J Cataract Refract Surg. 2018;44:541–56.









0 Comments